Fix the Hardware First: A Paradigm Shift in Acute and Chronic Traumatic Brain Injury Management
By Dr. Stefano Sinicropi, Founder of HyperCharge Health
Disclaimer: This blog is for informational purposes only and does not constitute medical advice. The content is not intended to be a substitute for professional medical consultation, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
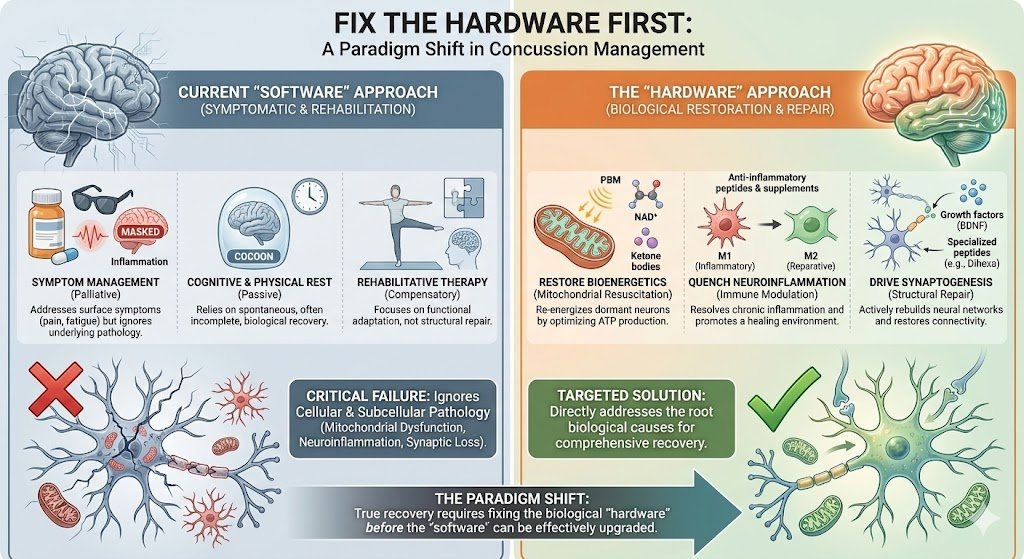
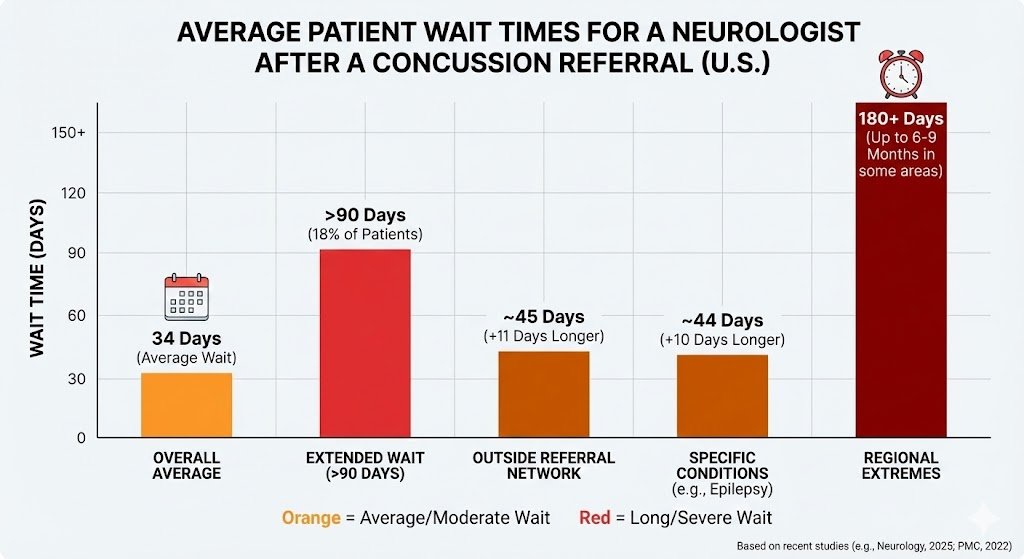
The standard of care for Traumatic Brain Injury (TBI) and concussion has long relied on a "software-centric" model: symptom management, cognitive rest, and rehabilitative therapy. However, this approach frequently fails to address the underlying "hardware" failure—the cellular and subcellular pathology resulting from the neurometabolic cascade of injury. Furthermore, with average wait times for neurology specialists now exceeding a month, patients are often losing the critical window for immediate repair, allowing acute injuries to calcify into chronic Post-Concussion Syndrome (PCS).
This review proposes a paradigm shift toward "Hardware Restoration." We begin by rejecting "normal" standard imaging in favor of objective functional diagnostics like EYEBOX tracking, Quantitative EEG (BrainView), and metabolic imaging (SPECT/PET). We then move to repair by targeting mitochondrial dysfunction, chronic neuroinflammation, glymphatic stasis, and synaptic loss through multimodal bio-interventions—specifically advanced Photobiomodulation, ketogenic metabolic switching, electromagnetic field therapies, and targeted peptide supplementation. Only once the biological hardware is stabilized can the software of cognition truly be upgraded.
The Unfortunate Cost of Waiting to Treat
If you dropped a high-performance laptop, shattering the motherboard and severing internal connections, you would not attempt to fix it by installing a new operating system. You certainly wouldn’t put it on a shelf for a month, hoping the circuits would fuse back together on their own. You would repair the hardware immediately.
Yet, in the field of neurology and concussion management, we have spent decades attempting to run high-performance software (complex cognition, emotional regulation, and motor control) on broken hardware. The current standard of care—often characterized by the "cocoon therapy" of dark rooms and gradual return to activity—relies heavily on the brain’s spontaneous recovery mechanisms.
This model is failing two distinct groups of patients:
The Acute Patient: Recent data indicates that the average wait time for a new patient appointment with a neurologist in the United States is approximately 34 days, with nearly 20% of patients waiting longer than 90 days [1]. For a brain suffering from an acute metabolic crisis, this delay is catastrophic. We are wasting the most critical biological window for repair while patients sit in dark rooms waiting for a consultation.
The Chronic Patient: Perhaps more tragic is the patient who suffered a concussion months or years ago and is told they have reached a "clinical plateau." They are told their headaches, brain fog, and fatigue are permanent because their MRI is "normal."
This is a false premise. The "Hardware First" model posits that chronic symptoms are not the result of permanent brain death, but of persistent, treatable biological dysfunction. Whether the injury occurred yesterday or five years ago, if the mitochondria are dormant and the inflammation is active, the hardware can be fixed.
The Invisible Injury: Why Your MRI is "Normal"
One of the most gaslighting experiences for a TBI patient is being told, "Your MRI looks clear." Standard CT and MRI scans are designed to detect gross structural damage—bleeding or skull fractures. They do not see inflammation, mitochondrial failure, or altered electrical activity. To fix the hardware, we must first use tools capable of seeing the microscopic faults.
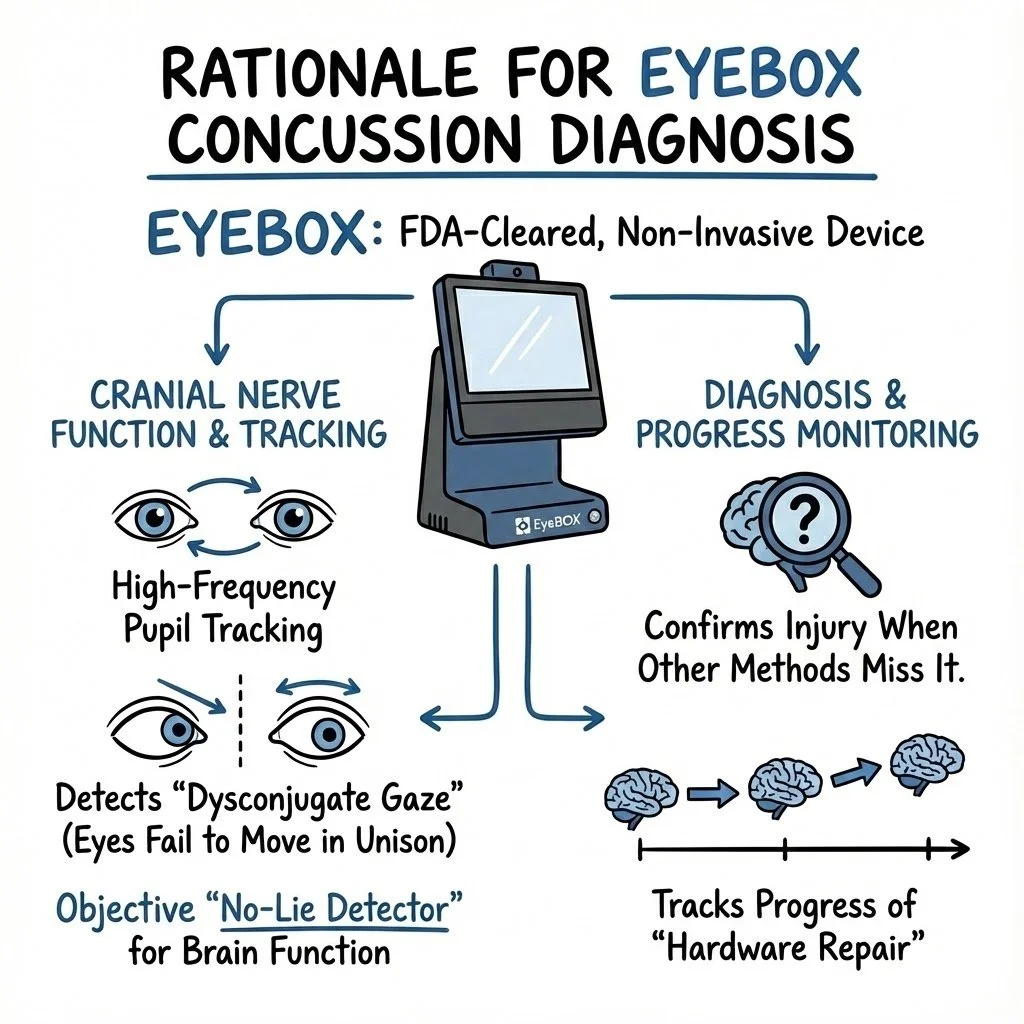
The Gold Standard for Cranial Nerves: EYEBOX Assessment
The brain controls eye movement through a complex network involving multiple cranial nerves (III, IV, and VI). When the "hardware" of the brainstem or midbrain is damaged, eye tracking becomes subtly erratic.
The Technology: We utilize the EYEBOX, the first FDA-cleared, non-invasive device for diagnosing concussion via cranial nerve function. Unlike a human observer, the EYEBOX tracks pupil movement at high frequency to detect "dysconjugate gaze"—where the eyes fail to move in perfect unison. It is an objective "no-lie detector" for brain function [2].
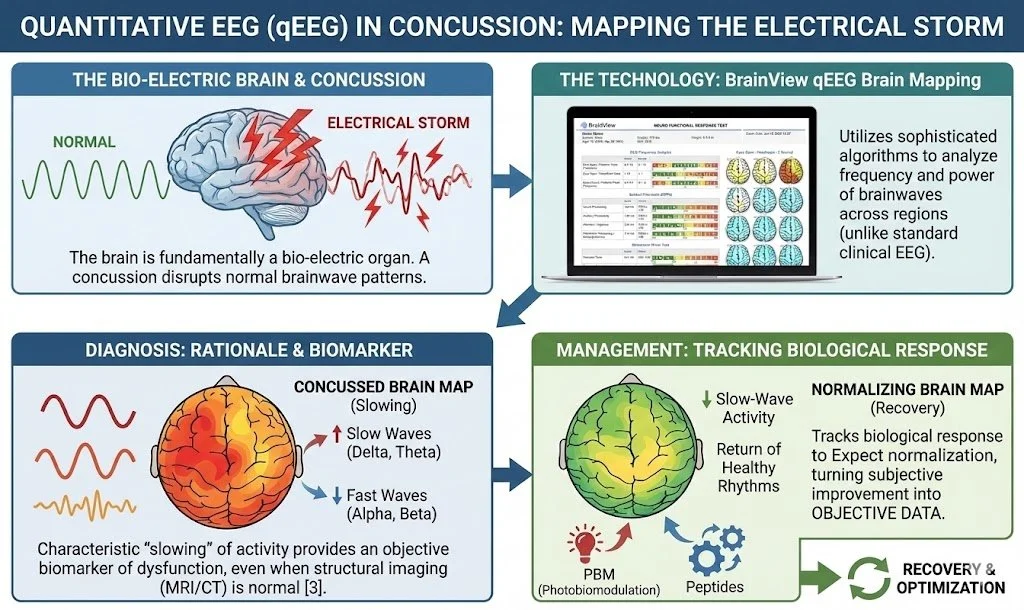
Mapping the Electrical Storm: Quantitative EEG (qEEG)
The brain is fundamentally a bio-electric organ. A concussion is an "electrical storm" that disrupts normal brainwave patterns.
The Technology (BrainView): We utilize the BrainView system to perform Quantitative EEG (qEEG) brain mapping. Unlike a standard clinical EEG used to detect seizures, qEEG employs sophisticated algorithms to analyze the frequency and power of brainwaves across different regions.
Rationale in Concussion:
Diagnosis: A concussed brain often shows a characteristic "slowing" of brainwave activity—an increase in slow Delta and Theta waves and a decrease in fast Alpha and Beta waves in specific cortical areas. This provides an objective biomarker of dysfunction even when structural imaging is normal [3].
Management: qEEG allows us to track the biological response to our therapies. As we repair the hardware with PBM or peptides, we expect to see a normalization of the brain map—a reduction in slow-wave activity and a return of healthy, organized rhythms. It turns subjective symptom improvement into objective data.
Advanced Imaging for Complex Cases: SPECT and PET
For patients with profound, resistant, or chronic symptoms, we look at blood flow and metabolism.
SPECT (Single Photon Emission Computed Tomography): Visualizes areas of hypoperfusion (low blood flow) that correlate with specific cognitive deficits.
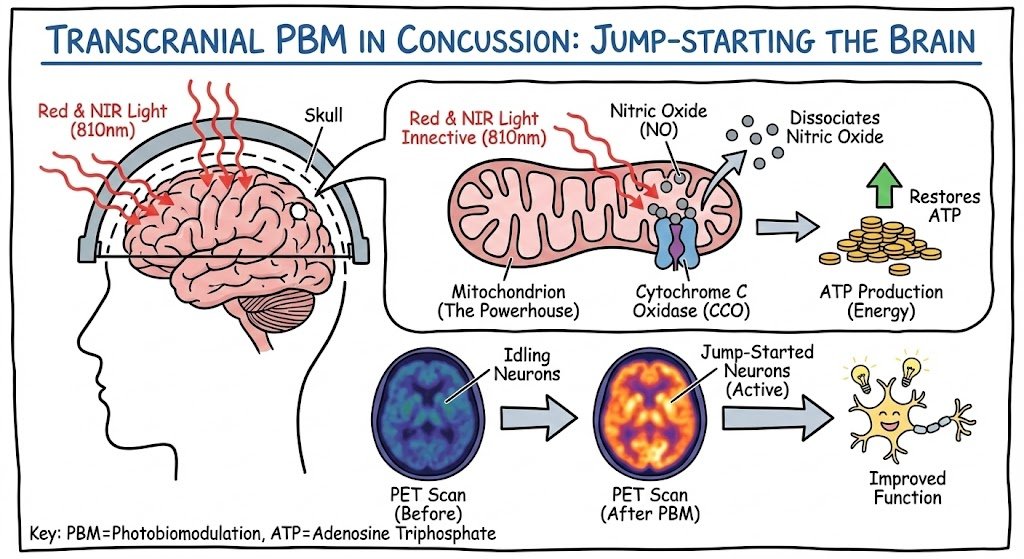
PET (Positron Emission Tomography): Visualizes glucose metabolism. In TBI, areas often show "hypometabolism"—confirming they are physically there but are starving [4].
The Pathophysiology: Why the Injury Persists
To fix the machine, we must understand the breakage. A concussion is a complex neurometabolic cascade.
The Energy Crisis (Mitochondrial Dysfunction)
Upon impact, neuronal membranes stretch, causing an indiscriminate flux of ions. This triggers a massive demand for ATP to restore homeostasis just as cerebral blood flow is often restricted. The result is an "energy crisis." In chronic cases, neurons enter a state of metabolic depression—they are dormant, "idling" cells [5].
The Fire That Never Goes Out (Chronic Neuroinflammation)
Microglia, the brain's immune cells, shift to a pro-inflammatory M1 phenotype to clear debris. In many patients, these cells remain "primed," releasing cytokines (IL-1β, TNF-α) indefinitely. This is why a minor stressor can trigger a massive symptom flare-up years later [6].
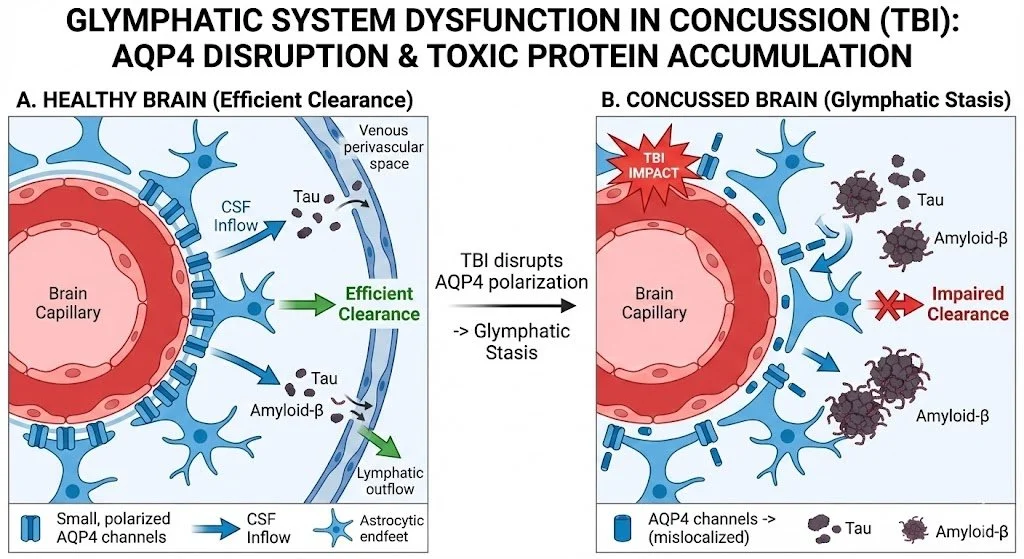
Glymphatic Stasis
TBI disrupts the polarization of Aquaporin-4 (AQP4) channels, leading to "glymphatic stasis." The brain cannot clear its own waste, leading to the accumulation of toxic proteins (Tau, Amyloid) [7].
The Light Revolution: Advanced Photobiomodulation
We cannot rebuild a house without electricity. The most potent tool for restoring the "power supply" to the neuronal motherboard is Photobiomodulation (PBM).
Transcranial PBM (tPBM): Waking the Dormant
Mechanism: Red and Near-Infrared (NIR) light (810nm) penetrates the skull and is absorbed by Cytochrome C Oxidase in the mitochondria. This dissociates Nitric Oxide and restores ATP production. It effectively "jump starts" the idling neurons identified on PET/qEEG [8].
Whole Body PBM: The Systemic Reset
Treating the head alone is insufficient. Whole Body PBM (light beds) treats the entire circulation, utilizing the abscopal effect to lower the total inflammatory load on the body, signaling the brain to downregulate its immune response [9].
Green Light Therapy: The Neural Modulator
While Red/NIR light targets the mitochondria, Green Light (520 nm) targets the sensory processing centers.
Mechanism: Green light targets Intrinsically Photosensitive Retinal Ganglion Cells (ipRGCs) which project to the thalamus. It produces smaller electrical potentials in the thalamus, effectively "turning down the volume" on central sensitization. It is a critical tool for post-traumatic headache and photophobia [10].
Metabolic Switching: The Ketogenic Advantage
We have established that the TBI brain suffers from an inability to process glucose efficiently (hypometabolism). However, the brain has a "hybrid engine."
The Ketogenic Solution: By adopting a ketogenic diet or utilizing exogenous ketone esters, we provide the brain with Beta-Hydroxybutyrate (BHB). BHB bypasses the broken glycolytic pathways and enters the mitochondria directly to produce ATP. It is a cleaner-burning fuel that lowers oxidative stress while keeping the lights on while the grid is being repaired [11].
Chemical Substrate: Orthomolecular Support
We must provide the raw materials for repair.
NAD+ Optimization: TBI depletes NAD+, a critical coenzyme for ATP production. Supplementation (IV or precursors) restores the redox ratio [12].
Creatine Monohydrate: A spatial energy buffer that maintains ATP levels during ischemic events [13].
N-Acetyl Cysteine (NAC): The precursor to Glutathione, scavenging free radicals [14].
Vitamin D3: A neurosteroid that regulates Nerve Growth Factor (NGF) [15].
Synaptogenesis: Rewiring the Circuitry
The most exciting frontier is synaptogenesis—using peptides to force the brain to grow new connections.
The Peptide Protocols
Semax: Rapidly elevates BDNF and NGF expression in the hippocampus, aiding memory reintegration [16].
Selank (The "Hardware Stabilizer"): In TBI, anxiety and stress prevent healing. Selank modulates GABA receptors and enkephalins, reducing the chronic stress response while boosting BDNF and modulating IL-6. It stabilizes the board so other components can be fixed [17].
Dihexa: A peptide derived from angiotensin IV, Dihexa is markedly more potent than BDNF at inducing synaptogenesis. It physically reconstructs dendritic spines [18].
BPC-157: Targets the gut-brain axis and repairs blood-brain barrier permeability [19].
A Note on Safety and Sequencing: While potent, these peptides are not "magic bullets." We utilize a Phased Protocol: Phase 1 focuses on extinguishing inflammation (BPC-157, Selank, NAD+), while Phase 2 focuses on aggressive growth (Dihexa, Semax). This "prepare the soil before planting" approach maximizes neuroplasticity and safety.
Electrophysiology: Tuning the Frequency
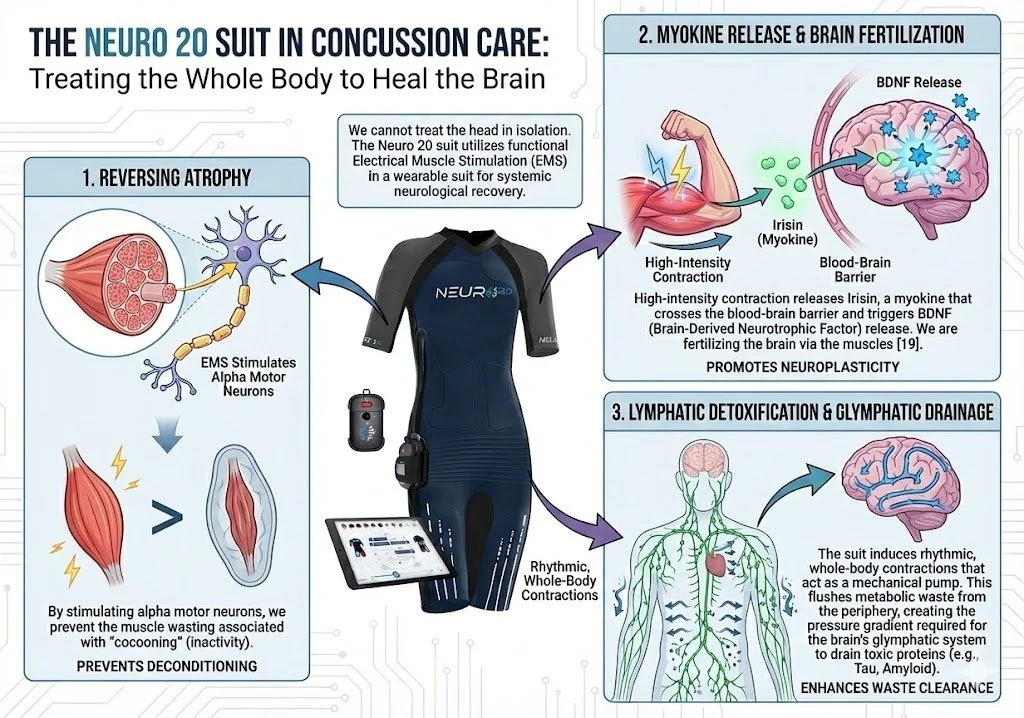
The Neuro 20 Suit: Whole-Body Neuromodulation
We cannot treat the head in isolation. The Neuro 20 suit utilizes functional Electrical Muscle Stimulation (EMS) in a wearable suit.
Reversing Atrophy: By stimulating alpha motor neurons, we prevent the muscle wasting associated with "cocooning."
Myokine Release: High-intensity contraction releases Irisin, a myokine that crosses the blood-brain barrier and triggers BDNF release. We are fertilizing the brain via the muscles [20].
Lymphatic Detoxification: The suit induces rhythmic, whole-body contractions that act as a mechanical pump. This flushes metabolic waste from the periphery, creating the pressure gradient required for the brain’s glymphatic system to drain toxic proteins.
Upgrading the Software
The model I have outlined here treats the brain not as a "black box" of psychology, but as a biological machine.
We start with objective truth (EYEBOX/qEEG). We stop the energy leak (Mitochondria/Ketones). We put out the fire (Inflammation/PBM). We clear the debris (Glymphatics/Neuro20). And finally, we rebuild the wires (Peptides).
Only after we have fixed this hardware does the "software" work become effective. By fixing the hardware first, we make the vestibular therapist’s job easier and the psychologist’s work more effective. We create a brain that is actually capable of learning from the therapy.
By utilizing these advanced modalities, we are not just managing symptoms; we are inducing neuro-restoration. We are building a better brain than the one that was injured.
Selected Bibliography
Lin, C. C., et al. (2025). "Wait Time to See a Neurologist After Referral." Neurology, 104(3).
Samadani, U., et al. (2015). "Detection of third and sixth cranial nerve palsies... eye tracking." Journal of Neurosurgery, 122(3), 707-720.
Thatcher, R. W., et al. (2001). "EEG discriminant analyses of mild traumatic brain injury." Electroencephalography and Clinical Neurophysiology, 73(2), 93-106.
Byrnes, K. R., et al. (2014). "FDG-PET imaging in mild traumatic brain injury: a critical review." Frontiers in Human Neuroscience, 7, 938.
Giza, C. C., & Hovda, D. A. (2014). "The new neurometabolic cascade of concussion." Neurosurgery, 75(S4).
Kumar, A., & Loane, D. J. (2012). "Neuroinflammation after traumatic brain injury." Brain, Behavior, and Immunity, 26(8).
Iliff, J. J., et al. (2012). "A paravascular pathway facilitating CSF flow." Science, 4(147).
Hamblin, M. R. (2016). "Photobiomodulation for traumatic brain injury and stroke." Journal of Neuroscience Research, 96(4).
Naeser, M. A., et al. (2014). "Significant improvements in cognitive performance post-transcranial, red/near-infrared LED therapy." Journal of Neurotrauma, 31(11).
Martin, L. F., et al. (2021). "Evaluation of Green Light Exposure on Headache Frequency." Cephalalgia, 41(2).
Prins, M. L., & Matsumoto, J. H. (2014). "The collective therapeutic potential of cerebral ketone metabolism in traumatic brain injury." Journal of Lipid Research, 55(12).
Klimova, N., & Kristian, T. (2019). "NAD+ depletion in brain injury." Translational Neuroscience.
Sakellaris, G., et al. (2006). "Prevention of traumatic headache with creatine." Acta Paediatrica.
Hoffer, M. E., et al. (2013). "Amelioration of acute sequelae of blast induced mild TBI by NAC." PLoS One.
Lawrence, D. W., & Sharma, B. (2016). "A review of the neuroprotective role of vitamin D." Journal of Neurosurgery.
Medvedeva, E. V., et al. (2014). "The peptide Semax affects the expression of genes." BMC Genomics.
Semenova, T. P., et al. (2010). "Comparison of the effects of Selank and tuftsin." Neuroscience and Behavioral Physiology.
McCoy, A. T., et al. (2013). "Evaluation of metabolically stabilized angiotensin IV analogs." J Pharmacol Exp Ther.
Sikiric, P., et al. (2018). "Brain-gut Axis and Pentadecapeptide BPC 157." Current Neuropharmacology.
Pedersen, B. K. (2019). "Physical activity and muscle-brain crosstalk." Nature Reviews Endocrinology.