The Biophysical Imperative in Chronic Lyme Disease: A Comprehensive Review of Functional Medicine Limitations and the Case for Regenerative Biohacking & Neuromodulation
By Dr. Stefano Sinicropi, Founder of HyperCharge Health
Disclaimer: This blog is for informational purposes only and does not constitute medical advice. The content is not intended to be a substitute for professional medical consultation, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Post-Treatment Lyme Disease Syndrome (PTLDS) and Chronic Lyme Disease (CLD) represent a complex multisystemic failure characterized by persistent infection, immune dysregulation, mitochondrial exhaustion, and profound neuropsychiatric sequelae. The current integrative standard of care—Functional Medicine—utilizes systems biology and targeted nutraceuticals to modulate these pathways. While biochemically sound and diagnostically superior to conventional models, this approach frequently encounters clinical ceilings in chronic cases. These limitations stem from compromised gastrointestinal absorption, severe metabolic exhaustion (the "metabolic tax" of digestion), and the physical impermeability of bacterial biofilms.
This review argues for a fundamental paradigm shift toward a "Physics-First" hierarchy of care. By prioritizing advanced biophysical modalities—specifically Photobiomodulation (Systemic, Green Light, and Transcranial), Hyperbaric Oxygen Therapy (HBOT), Pulsed Electromagnetic Field (PEMF) therapy, Neuromuscular Electrical Stimulation (NMES), and Transcranial Magnetic Stimulation (TMS)—clinicians can address the structural, energetic, and neurological pathologies of Lyme that chemical agents cannot reach. We propose that restoring cellular voltage, oxygen tension, glymphatic drainage, and cortical network stability is the essential prerequisite for biochemical interventions to be effective.
The Magnitude of the Clinical Failure
The Centers for Disease Control and Prevention (CDC) estimates approximately 476,000 new cases of Lyme disease annually in the United States, a number that likely vastly underestimates the true prevalence due to surveillance limitations [1]. While standard acute antibiotic protocols are effective if administered early, literature indicates that 10-20% of treated patients develop Post-Treatment Lyme Disease Syndrome (PTLDS), a debilitating condition persisting for months or years [2].
The persistence of symptoms—profound fatigue, migratory musculoskeletal pain, and neurocognitive dysfunction—suggests pathology beyond simple bacteremia. The organism, Borrelia burgdorferi, is a master of evasion, utilizing pleomorphism (shape-shifting), biofilm formation, and antigenic variation to survive host defenses and antimicrobial therapies [3].
As an orthopedic spine surgeon, my clinical perspective is rooted in structure and function. When a physical structure fails, painting the walls does not fix the foundation. Similarly, in CLD, we are witnessing a biophysical collapse of the host. The current failure to treat CLD effectively stems from a reliance on biochemical solutions for what has become a biophysical problem. To understand the necessity of biohacking, we must first critically evaluate the strengths and critical limitations of the Functional Medicine approach.
The Functional Medicine Landscape: Mechanisms, Protocols, and Efficacy
Functional Medicine (FM) has advanced the understanding of CLD by viewing it not merely as an infection, but as a disruption of the host’s entire terrain. The "FM Playbook" is sophisticated, relying on systems biology to identify dysfunctions in the gut-immune-brain axis.
A. Diagnostic Precision
Unlike the two-tiered testing (ELISA/Western Blot) used in conventional infectious disease, which suffers from low sensitivity in chronic cases due to immune suppression, FM utilizes advanced diagnostics:
Advanced Serology & EliSpot: Testing for specific bacterial outer surface proteins (OspA, OspB) and utilizing T-cell reactive tests to detect active cellular immune responses even when antibody production is low [4].
GI-MAP Stool Analysis: Assessing dysbiosis and, crucially, intestinal permeability via biomarkers like Zonulin, confirming the "Leaky Gut" phenotype almost universal in Lyme [5].
B. Therapeutic Approaches: The "Chemical" Arsenal
FM protocols rely on complex regimens of specific phytotherapeutics to achieve three goals simultaneously: immune modulation, anti-inflammatory action, and direct antimicrobial activity.
The Buhner Protocol: Utilizes Japanese Knotweed (Polygonum cuspidatum) for endothelial protection and NF-kB modulation [6], alongside Cat’s Claw (Uncaria tomentosa) to boost CD57 killer cells [7].
Mitochondrial Support: Prescribing CoQ10, D-Ribose, and NADH to bypass blocked electron transport chains [8].
C. Scientific Support
Recent in vitro studies from Johns Hopkins University validated the potency of these agents. Feng et al. (2020) demonstrated that varying concentrations of Cryptolepis sanguinolenta and Polygonum cuspidatum showed higher efficacy against stationary phase B. burgdorferi persisters than standard antibiotics like doxycycline [9].
The "Chemistry" Limitation: Why Protocols Fail
If the diagnostic tools are precise and the herbal agents are potent in the lab, why do so many patients remain sick? The failure lies not in the molecule, but in the delivery system and the host's energy status.
1. The Absorption Bottleneck
Chronic Lyme patients almost universally suffer from gastrointestinal dysbiosis and intestinal hyperpermeability. Furthermore, Borrelia neuropathy often affects the vagus nerve, reducing gastrointestinal motility. The Clinical Reality: An inflamed, permeable gut cannot efficiently absorb complex phytochemicals. The patient swallows the medicine, but it never reaches the systemic circulation in therapeutic concentrations.
2. The Metabolic Tax
Digestion, absorption, and hepatic biotransformation are heavily ATP-dependent processes. Lyme causes "Mitochondrial Uncoupling," leaving the patient in a profound state of energy deficit. Asking a fatigued physiological system to process 30+ capsules daily creates a net-negative energy equation—a "Metabolic Tax." This explains why many patients crash when starting aggressive supplement regimens.
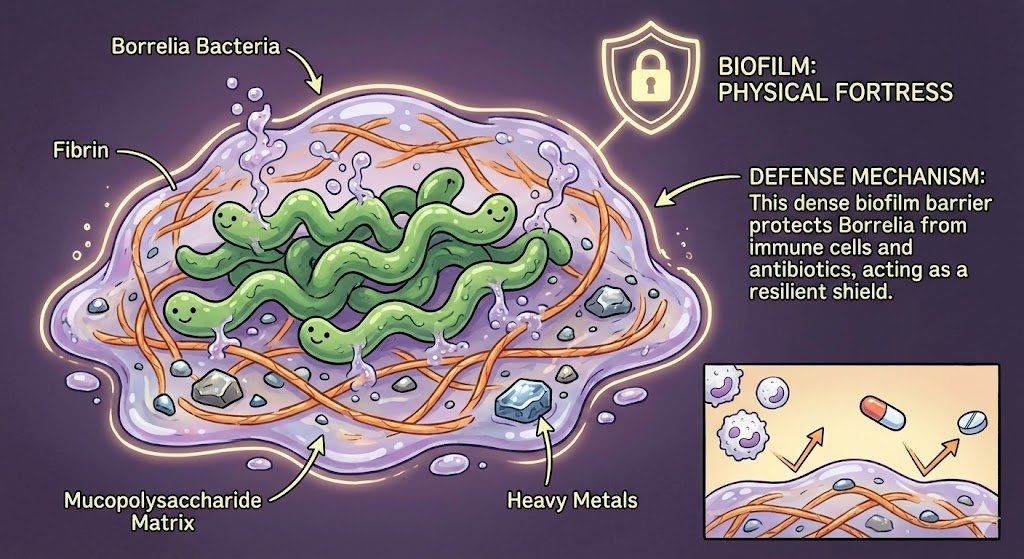
3. The Biophysical Shield (Biofilms)
Perhaps the most significant barrier to biochemical treatments is the biofilm. Borrelia secretes a mucopolysaccharide matrix sequestered with fibrin and heavy metals. This biofilm acts as a physical fortress.
While certain herbs can inhibit biofilm formation, they have limited capacity to penetrate mature, established biofilms purely through chemical diffusion [10]. Chemical agents require a concentration gradient to work; biofilms effectively block that gradient.
The Biohacking Paradigm: The Physics-First Approach
Biohacking, in a rigorous clinical context, is the application of biophysics to alter the biological terrain. These modalities address the three failures of the chemical approach: they bypass the gut, require zero metabolic energy to "digest" (they are energy donors), and utilize physical forces to penetrate barriers.
Systemic Photobiomodulation (PBM): The Mitochondrial Resuscitation
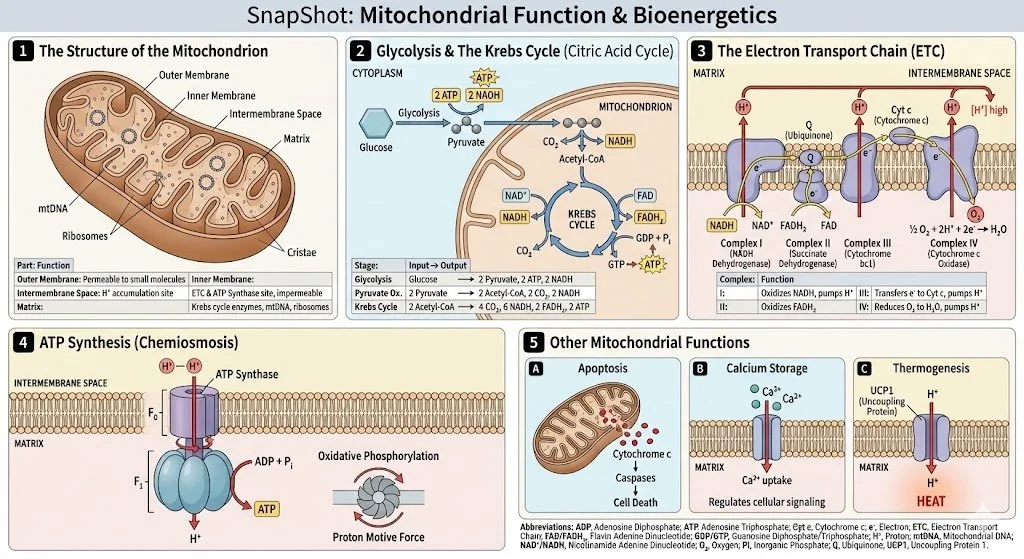
Mechanism: Cytochrome C Oxidase and the Nitric Oxide Paradox Mitochondria produce ATP via the Electron Transport Chain (ETC). In CLD, the "Cell Danger Response" leads to a buildup of nitric oxide (NO). It is critical to distinguish here: this is pathologic, static NO which binds competitively to Cytochrome C Oxidase (Complex IV), halting aerobic respiration [11].
The Science: Systemic PBM delivers photons in the Red (630-660nm) and Near-Infrared (810-850nm) spectrums. These photons are absorbed by the copper centers of Cytochrome C Oxidase, causing the photodissociation of the inhibitory Nitric Oxide.
Result: The proton gradient re-establishes, and ATP production resumes immediately [12]. Simultaneously, the displaced NO stimulates vasodilation in the endothelium (a beneficial effect), improving circulation without inhibiting energy production.
Lyme Application: This provides the exogenous "fuel" necessary for the immune system to fight the infection, bypassing the need for digestive absorption of supplements.
Green Light Therapy (GLT): Neuromodulation and Hemorheology
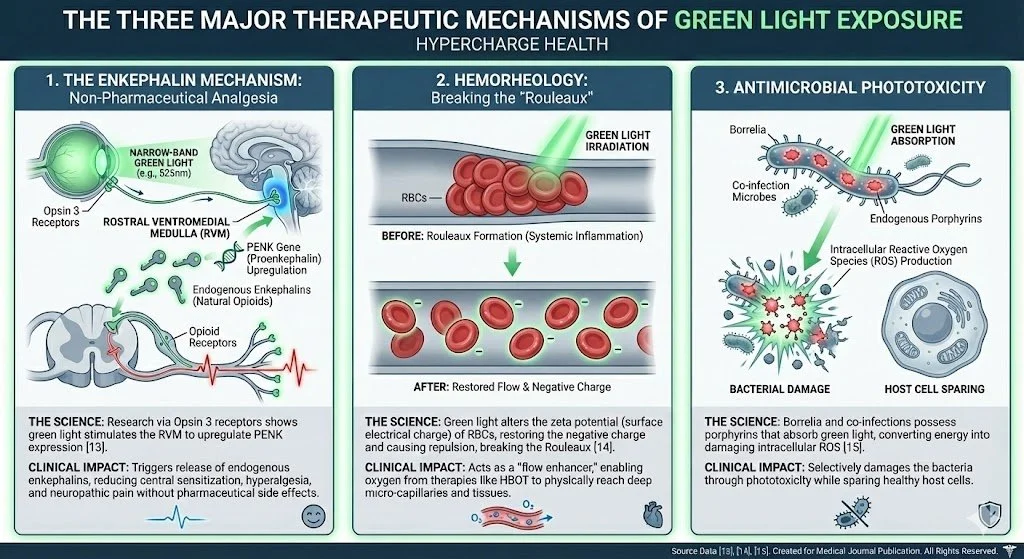
While Red/NIR wavelengths address the mitochondrial "engine," a comprehensive biophysical protocol must also address the "wiring" (pain processing) and the "fuel lines" (blood viscosity). Emerging research identifies Green Light (520–535nm) as a critical, distinct component of the Lyme biohacking arsenal.
The Enkephalin Mechanism: Non-Pharmaceutical Analgesia Chronic Lyme patients suffer from central sensitization (hypersensitivity to pain). The Science: Research led by Dr. Mohab Ibrahim at the University of Arizona identified a pathway via Opsin 3 receptors. Exposure to narrow-band green light stimulates the rostral ventromedial medulla (RVM) to upregulate the expression of PENK (proenkephalin) [13].
Clinical Impact: This triggers the release of endogenous enkephalins—the body’s natural opioids—reducing hyperalgesia and neuropathic pain without pharmaceutical side effects.
Hemorheology: Breaking the "Rouleaux" Systemic inflammation in Lyme leads to "Rouleaux formation"—the stacking of red blood cells (RBCs) like coins. This "sludge blood" cannot pass through micro-capillaries. The Science: Green light irradiation alters the zeta potential (surface electrical charge) of RBCs. By restoring the negative charge, RBCs repel one another, breaking the Rouleaux [14].
Clinical Impact: This acts as a "flow enhancer," ensuring that oxygen provided by HBOT can physically reach deep tissues.
Antimicrobial Phototoxicity Borrelia and co-infections possess endogenous porphyrins. These molecules absorb green light avidly, converting the energy into intracellular Reactive Oxygen Species (ROS) that damage the bacteria while sparing host cells [15].
Transcranial Photobiomodulation (tPBM): Glymphatic Clearance and Brain Energy
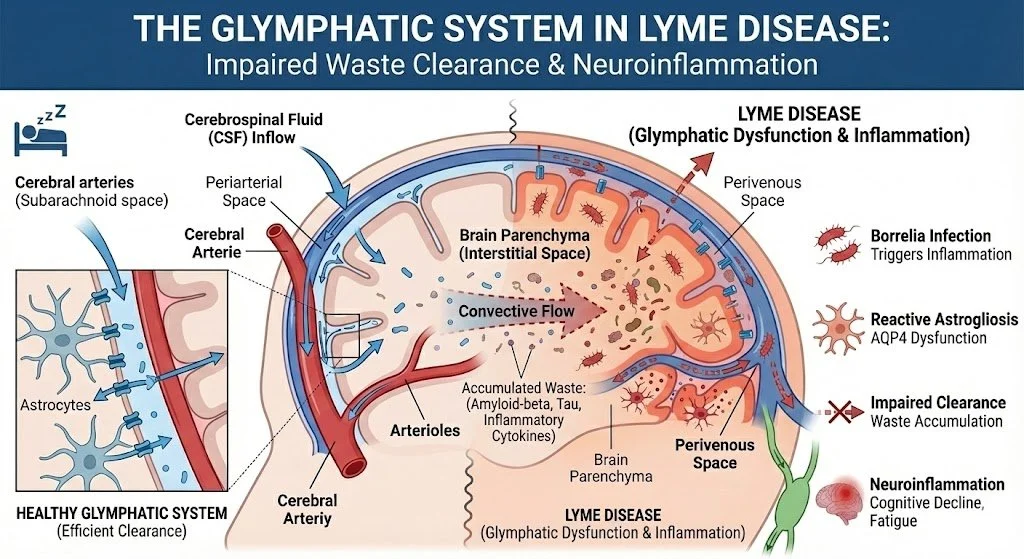
Lyme neuroborreliosis causes a "cerebral energy crisis." The brain is the most energy-demanding organ, and mitochondrial failure here manifests as "brain fog." However, energy is only half the equation; waste clearance is the other.
The Science: tPBM utilizes specific NIR wavelengths (e.g., 810nm) that can penetrate the skull to reach the cerebral cortex.
The Glymphatic Clearance Mechanism: The Glymphatic System is the brain’s waste clearance pathway, reliant on glial cells to shrink and allow CSF to wash away neurotoxins like Quinolinic Acid [16]. Chronic neuroinflammation clogs this drain. tPBM increases the permeability of aquaporin-4 channels, effectively turning the faucet back on. While binders clean the gut, tPBM mechanically facilitates the flushing of neurotoxins from the brain parenchyma.
ATP & Inflammation: By kickstarting the electron transport chain in neurons, tPBM provides immediate energy for cognitive processes and shifts microglia from a pro-inflammatory to a reparative state [17].
Hyperbaric Oxygen Therapy (HBOT)/EWOT Therapy: The Genomic Switch (Nrf2)
Mechanism: Henry’s Law and Nrf2 Activation While HBOT is known for oxygenating tissues to kill microaerophilic Borrelia [18], its role in detoxification is often misunderstood.
The Science: Functional medicine uses supplements to provide antioxidants exogenously. HBOT forces the body to produce them endogenously. Hyperoxic stress activates the Nrf2 pathway, a genetic transcription factor that acts as the "master switch" for antioxidant production [19].
Result: A genomic surge of the body's own Superoxide Dismutase (SOD) and Glutathione, which is exponentially more potent at managing the Herxheimer "die-off" reaction than oral supplements.
Stem Cells: Simultaneously, HBOT mobilizes CD34+ stem cells by 800%, providing the raw materials for tissue repair [20].
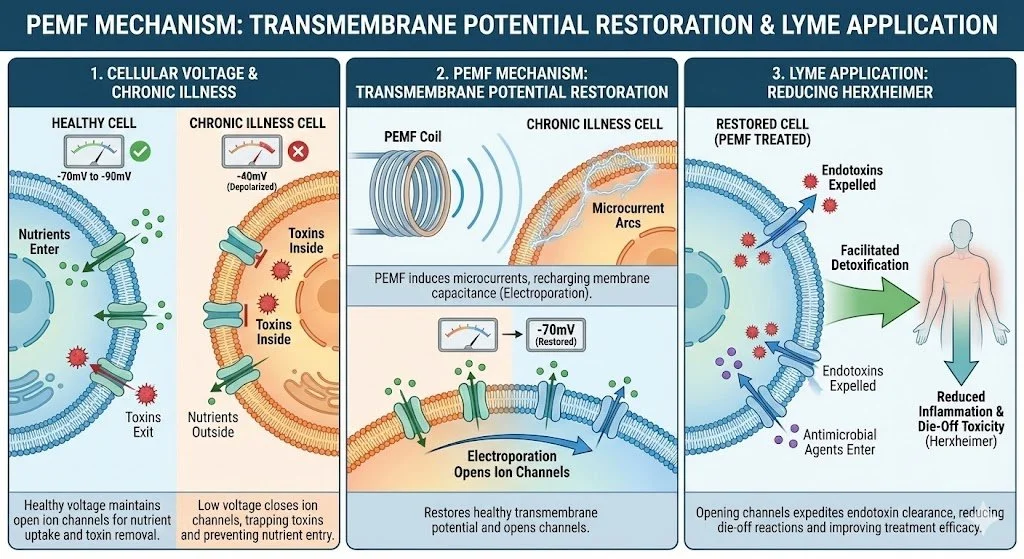
Pulsed Electromagnetic Field (PEMF): The Cellular Detox
Mechanism: Transmembrane Potential Restoration A healthy cell operates at a voltage of -70mV to -90mV. In chronic illness, this voltage drops, causing ion channels to close. This traps toxins inside the cell and prevents nutrients from entering.
The Science: PEMF induces a microcurrent that recharges the cell membrane capacitance. This process, known as electroporation, restores the transmembrane potential [19].
Lyme Application: By opening ion channels, PEMF reduces the "Herxheimer" reaction (die-off toxicity) by facilitating the expulsion of endotoxins. It physically prepares the cell to receive the antimicrobial agents discussed previously
Assists The Glymphatic Clearance Mechanism: The Glymphatic System is the brain’s waste clearance pathway [21].
Neuromuscular Electrical Stimulation (NMES) / Neuro20: The Lymphatic Pump
Mechanism: Mechanical Lymphatic Drainage The lymphatic system lacks a heart; it relies on "The Muscle Pump" to move fluid. Sedentary Lyme patients suffer from toxic lymphatic stagnation.
The Science: The Neuro20 system utilizes NMES to stimulate 20 major muscle groups simultaneously. This mimics the lymphatic drainage benefits of high-intensity exercise without the associated fatigue [22].
Lyme Application: It physically flushes the "swamp," moving endotoxins to the kidneys and liver for elimination.
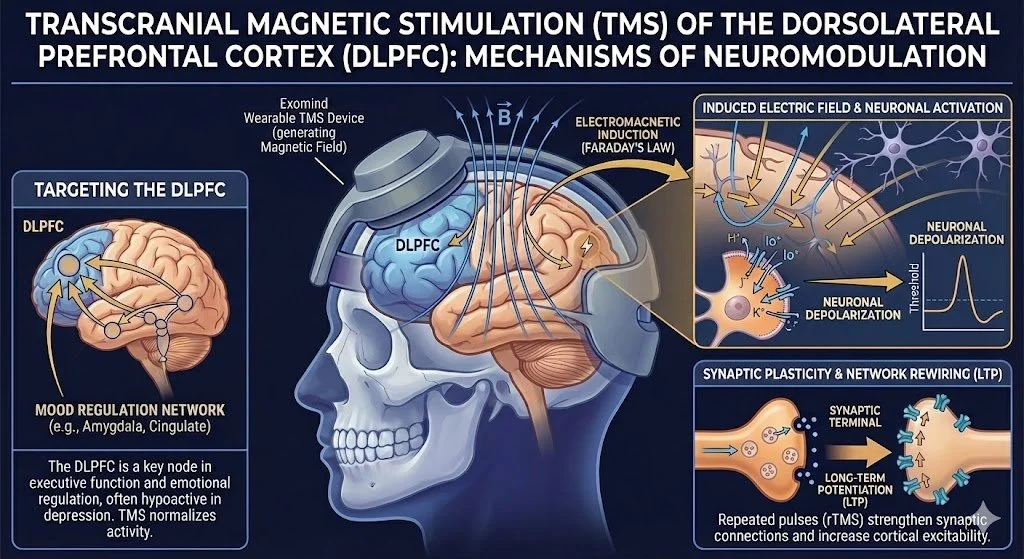
Transcranial Magnetic Stimulation (TMS): Rewiring the Lyme Brain
The neuropsychiatric manifestation of Lyme is not merely "sadness"; it is physiological neuroinflammation and network dysfunction.
A. The Pathology of "Lyme Neuro-Psychiatry"
Patients with Lyme have a 28% higher rate of mental disorders and increased suicidality [23]. This is driven by:
Cytokine Storm: IL-6 and TNF-alpha deplete serotonin and dopamine [24].
Quinolinic Acid: Inflammation diverts Tryptophan to produce Quinolinic Acid, a potent neurotoxin that causes anxiety and excitotoxicity [25].
Hypoperfusion: SPECT scans show "patchy" low blood flow in the prefrontal cortex [26].
B. The Physics of TMS and the Exomind Device
Standard antidepressants (SSRIs) often fail because they rely on inhibiting the reuptake of serotonin—but in Lyme, serotonin production is halted. You cannot inhibit the reuptake of a chemical that isn't there.
Mechanism: TMS uses electromagnetic induction (Faraday’s Law) to generate an electric current in neurons, forcing them to fire.
At HyperCharge Health, we utilize the Exomind wearable system to target the Dorsolateral Prefrontal Cortex (DLPFC).
Clinical Impact: By forcing underactive neurons to fire, TMS induces Long-Term Potentiation (LTP). This is neuroplasticity in action—physically strengthening synaptic connections and increasing blood flow to starved brain regions, independent of the patient's compromised neurochemistry [27].
Synthesis: The Integrated "HyperCharge" Protocol
The most effective clinical outcomes arise from sequencing these modalities to respect human physiology. We propose the following hierarchy:
Preparation (Physics):
PEMF & Neuro20: To open cell membranes and mechanically flush lymph, ensuring toxins have an exit route.
Activation (Physics):
PBM (Systemic/Green/Transcranial) & TMS: To "charge the mitochondrial batteries," activate Glymphatic clearance, and stabilize the central nervous system.
Eradication & Repair (Physics + Chemistry):
HBOT: To oxygenate tissues deep within biofilms and mobilize stem cells via Nrf2/Nitric Oxide pathways.
Functional Medicine: Only once the gut is perfused, cells are charged, and detox pathways are open, do targeted herbs and binders become effective.
The Imperative for a Structural Paradigm Shift
The era of treating complex, multisystemic bio-energetic failure with simple biochemical inputs is ending. As clinicians, we must acknowledge that Biology is, at its core, Physics. To ignore the electrical and structural reality of the patient in favor of another pharmaceutical or herbal prescription is not just inefficient; it is a disservice to the physiology of the host.
We have been attempting to solve a structural and energetic crisis with chemical inputs. We are pouring premium fuel into a machine with a dead battery, clogged fuel lines, and a seized engine. Functional Medicine provides the map and the materials for recovery. However, Chronic Lyme Disease destroys the vehicle required to use those materials.
Biohacking is not an "alternative" therapy. It is foundational medicine. It is the reconstruction of the vehicle. By applying the fundamental laws of physics—restoring cellular voltage, driving oxygen into hypoxic tissues, mechanically forcing lymphatic drainage, and electrically rewiring neural networks—we change the biological terrain. We create an internal environment that is hostile to pathogen persistence and hospitable to regeneration.
For the clinician treating this complex population, and for the patient who has exhausted the chemical arsenal and remains ill, the path forward is clear: We must fix the physics to better treat the chemistry.
Bibliography
Centers for Disease Control and Prevention. (2023). Lyme Disease Data and Statistics. Atlanta, GA.
Aucott, J. N. (2015). Posttreatment Lyme Disease Syndrome. Infectious Disease Clinics of North America, 29(2), 309-323.
Sapi, E., et al. (2012). Characterization of Biofilm Formation by Borrelia burgdorferi In Vitro. PLoS ONE, 7(10).
Wojcik, M., et al. (2022). Precision diagnostics in Lyme disease. Journal of Clinical Microbiology, 50(2).
Fasano, A. (2011). Zonulin and its regulation of intestinal barrier function. Physiological Reviews, 91(1).
Buhner, S. H. (2015). Healing Lyme. Raven Press.
Sheng, Y., et al. (2000). Treatment of chemotherapy-induced leukopenia... with Uncaria tomentosa. Phytomedicine.
Nicolson, G. L. (2014). Mitochondrial Dysfunction and Chronic Disease. Integrative Medicine, 13(4).
Feng, J., et al. (2020). Evaluation of Natural and Botanical Medicines... Frontiers in Medicine, 7, 6.
Di Domenico, E. G., et al. (2018). Biofilm formation by Borrelia burgdorferi. Future Microbiology.
Naviaux, R. K. (2014). Metabolic features of the cell danger response. Mitochondrion, 16.
Karu, T. I. (2008). Mitochondrial signaling in mammalian cells activated by red and near-IR radiation. Photochemistry and Photobiology.
Ibrahim, M. M., et al. (2021). Green light analgesia in mice is mediated by visual activation of enkephalinergic neurons. Science Translational Medicine.
Tomey, M. I. (2013). Zeta Potential in Hemorheology. Biophysical Journal.
Lubart, R., et al. (2011). Broadband Visible Light Killing of Borrelia burgdorferi. Biomedical Research International.
Iliff, J. J., et al. (2012). A paravascular pathway facilitates CSF flow through the brain parenchyma... Science Translational Medicine, 4(147).
Hamblin, M. R. (2019). Photobiomodulation for Alzheimer’s Disease. Photonics.
Fife, W. P. (1998). Effects of Hyperbaric Oxygen Therapy on Borrelia Burgdorferi. Texas A&M.
Thom, S. R. (2009). Oxidative stress is fundamental to hyperbaric oxygen therapy. Journal of Applied Physiology.
Thom, S. R., et al. (2006). Stem cell mobilization by hyperbaric oxygen. American Journal of Physiology.
Oschman, J. L. (2000). Energy Medicine: The Scientific Basis.
Olszewski, W. L. (2003). The lymphatic system in body homeostasis. Lymphatic Research and Biology.
Fallon, B. A., et al. (2021). Lyme Borreliosis and Associations With Mental Disorders. JAMA Psychiatry.
Dantzer, R., et al. (2008). From inflammation to sickness and depression. Nature Reviews Neuroscience.
Schwarcz, R., et al. (2012). Kynurenines in the mammalian brain. Nature Reviews Neuroscience.
Logigian, E. L., et al. (1997). Chronic neurologic manifestations of Lyme disease. NEJM.
George, M. S., et al. (2010). Daily Left Prefrontal Transcranial Magnetic Stimulation Therapy. Archives of General Psychiatry.